29 year old female, sought treatment on 10-16-15 for liver failure due to alcohol use. She was sent home from the E.R. to receive hospice care. Following are the lab values for 3-2-15 to 5-17-16.
BEFORE TREATMENT:

M. is a 29 year old female status post emergency room visit for acute alcohol withdrawal. The patient was seen in the emergency department the evening of October 5th 2016, accompanied by her mother. She was discharged from the emergency department to home with an anti-seizure medication Librium and anti-emetic Promethazine. First, contact with patient was on October 6th 2016 in the patient’s home.
Patient complains of weakness, fatigue, and “feeling shaky”. She states that she knows “I am in alcohol withdrawal, because I have been through it many times before”.
Patient went to the emergency department because she was attempting to stop drinking alcohol. She began feeling very ill after 10 hours of abstaining and no longer felt like she was safe to be at home. R.M. expressed a desire to stop drinking multiple times according her mother and herself. She has had a seizure in the past while detoxing and did not want to go through that again and stated that she “was afraid of not coming out of the seizure and dying”. Physician in the E.D. according to the patients mother; expressed that there was nothing that the facility could do for the patient regarding R.M. ‘s health and liver status and that if she were to make it through this detoxification she would need hospice to prepare her for and keep her comfortable during end of life. This prognosis was due to lab finding and multiple admissions to facility for detoxification. The patient was then discharged to home with Librium and Promethazine. Early October 6th, 2016 VibrantLife of Oklahoma was contacted by the patient’s mother. Chiropractor/Naturopath specializing in detoxification, nutrition, vitamins and minerals made a house call to see R.M. and treatment was initiated that day.
Past medical and mental history was obtained by patients own recall. R.M. has a mental history of clinical depression. Medical history includes: morbid obesity, Charcot-Marie-Toothe, cholecystitis, alcoholism, liver failure, alcohol induced hepatitis, pancreatitis, gastrointestinal bleed at the duodenum requiring packed red blood cell, platelet, and albumin transfusion, mild varices of the esophagus and stomach, osteomyelitis of the right distal fibula, talus, tarsals, and metatarsals. Patient has also had a seizure induced by alcohol withdrawal delirium trements. She is gravida-0 and para-gravida-3. Patient is not currently on any daily medication, prior to what was prescribed to her in the emergency department.
Patient admits to being an alcoholic for greater than 5 years with intermittent periods of sobriety, none lasting longer than 3 months. In 2011, R.M. was admitted to the ICU and diagnosed with liver failure and 4% liver function. Patient spent 9 days in intensive care before being discharged to a residential facility in Cushing, Oklahoma for rehab. According to patient’s mother, patient was not medically stable or physically capable to participate in the rehabilitation program and was denied by the facility after arriving and initial assessment was done. After several days post discharge from the intensive care unit, the patient entered an outpatient rehabilitation program 3 times a week for the duration of the program which was 1 month. Per the patient, she resumed drinking substantial amounts of alcohol. Patient states that she would drink at least a quart of 100 proof vodka or 80 proof whiskey on a daily basis. She states that this was her normal amount prior to and after diagnosis of liver failure.
Patient’s surgical history begins with tonsillectomy and reduction of adenoids in 1990. She had Roux-en-Y gastric bypass in 2004 due to morbid obesity. In 2005, she had a cholecystectomy due to a blockage in the gall bladder duct. R.M. has had several elective surgeries which include bilateral brachioplasty, breast lift with augmentation, and abdominoplasty in 2007 due to excess skin post gastric bypass. In 2010, she has a dilation and curettage of her uterus following miscarriage at 13 weeks.
Family history is as follows. Paternal grand-father is living and has a history of colon cancer with colostomy placement, diabetes type II, kidney disease, triple bypass with pacemaker placement. He has a social history of alcoholism and tobacco use. Paternal grand-mother is deceased, 2003, due to septicemia caused by a diabetic ulcer. She has a history of morbid obesity, diabetes type II, diabetic neuropathy, Charcot-Marie-Toothe, histoplasmosis, macular-degeneration, hypertension, congestive heart failure, gravida 4 with 1 term stillbirth, and para-gravida 5. No social history. Father has a history of morbid obesity and hypertension both resolved with gastric bypass and clinical depression. He has a social history of alcoholism and tobacco use. Maternal grand-father is deceased, 2001, due to suicide post cancer diagnosis. His history includes paranoid schizophrenia, cancer of the trachea with mets throughout the body, and obesity. His social history includes occasional alcohol and tobacco use. Maternal grand-mother has mild hypertension and is overweight. She has a social history of social drinking in excess and tobacco use. Mother has a history of morbid obesity and hypertension resolved with gastric bypass, hypothyroidism, clinical anxiety, gravida 2 and para-gravida 4. Patients brother has no known medical or social history.
Patient is 29 years old and a high school graduate. She also has and Associates in Applied Science in Paramedic Technology and Associates in Applied Science Paramedic to Nursing Bridge. R.M.’s parents divorced at her age of 15. Both parents are re-married. She has one brother who is 8 years younger. Patient has 2 step-sisters and 1 step-brother on her fathers’ side. No step-siblings on mothers’ side. Patient is married with no children. Husband is an alcoholic with mild abusive verbal behavior when intoxicated. He has health issues including liver problems and multiple gastrointestinal bleeds and varices due to alcoholism, also use of tobacco products but, otherwise is healthy. They have been married for greater than 6 years. No physical abuse noted or reported. Patient and husband live and rent a 3 bedroom home in the country. Patient does the majority of the cooking, cleaning, shopping, and bill pay. Patient’s husband takes care of curtilage of house including yard work and trash responsibilities. Patient’s husband is currently un-employed; he was a medic for greater than 19 years on an ambulance. The two have no previous children or children together.
R.M. was a paramedic on an ambulance for several years before becoming a registered nurse. She worked in a local rural emergency department and then several years in the neurological intensive care unit beginning in January of 2011. During the time while working in the ICU is when the patient states that her drinking became more prominent and frequent. Also, during this time the patient was admitted to the ICU herself for liver failure in November of 2011. Once liver failure had stabilized out of the acute state the patient returned to the ICU as a RN. The patient then got osteomyelitis/avascular necrosis on her right foot and was put on medical leave of absence again, after two weeks the medical leave ran out and patient was forced to resign which caused termination of her health insurance in May of 2013. Patient was out of work for the majority of 2013 into 2014 with intermittent jobs in home health an outpatient surgery center before becoming a school nurse in June of 2014. Her position at the school was eliminated and her contract was not renewed for the following school year. In August of 2014, patient was hired as a nightshift supervisor at a long-tern acute care center. After, one month with no incidences or write-ups patient was terminated due to the accusation of stealing narcotics with two random drug screens administered by the facility that were negative. Patients states that she did not drink alcohol during her time at the facility or a month prior to beginning work. Patient states that she became very depressed after the loss of her job and she began to drink copious amounts of alcohol in late September 2014, leading to this appointment.
Upon initial assessment head, eyes, ears, nose and throat appear normal, with the exception of jaundice to sclera. Skin is intact with bruising in various spots in all stages of healing, no signs of physical abuse. Skin turgor is rapid, however most likely dehydrated due to nature of illness. She also has jaundice of the skin and nail beds. She is overweight and states that she currently weighs 210 pounds and is 5’11”. Patient’s nutrition status is difficult to determine, due to nausea and poor appetite at this time. Patient has moderate pitting edema in lower extremities, no ascits noted at this time. Patient has rebound tenderness upon palpation to upper right quadrant of abdomen. Patients gait is unsteady, patient states that she is shaky and weak. Tremors noted in patients hands. She is lethargic and often does not make sense when speaking.
Initiation of treatment began the morning of October 6th 2016. The patient was given intravenous therapy of vitamin C, magnesium, B-vitamins, and a separate dose of glutathione. Care in the patient’s mother’s home where the same treatment was done 2 times a day for 4 days. By day 5 or October 11th 2014 the patient was able to be seen in the clinic for her IV therapy. Patient was placed on a multitude of vitamins at home including: Liposomal C, L-Glutamine, 5-HTP, Magnesium, DL-Phenalinine, GABA, Omega-3 fish oil, Neuro-optimizer, SAM-E, thiamin, milk thistle, and melatonin. She was also put on a strict nutritional diet excluding all sugars (including fruit), carbohydrates, and dairy.
Patient was seen in the clinic daily for 3 months. In November 2015, patient received an implant of Naltrexone, however during the course of healing the area below the patients left hip where the implant was placed subcutaneously began to swell and become red and fluid filled. Patient reported that while getting dressed the area was pushed against and ruptured open releasing a moderate amount of puss, serosanguineous and sanguineous fluid. Multiple attempts to close wound using aseptic technique and steri-strips along with sterile dressings were made. Area continued to produce sanguineous fluid; during a dressing change de-hissed completely and the implant came out of the tissue still in capsule form. Despite the failure of the implant the patient visibly improved, jaundice subsided slowly over the 3 month course. Patient exhibited more energy and cognitively more aware with each day.
Patient treatments were decreased to 2 times a week for approximately 1 month. In mid-January 2016, patient began complaining of left hip discomfort. Over the next month patient received several manual adjustments and one injection with worsening of pain and discomfort. It was suggested to the patient that she obtain an MRI. On February 23rd 2016, patient was diagnosed with Avascular Necrosis of the hips, the left hip was staged at a IV and the right at a II. Two highly common reasons for this type of bone necrosis are a large amount of steroids over any amount of time, and alcoholism. During the patients first ICU stay she received Prednisone 160mg a day and was sent home on that amount without a tapering dose. Patient has been previously diagnosed with this in her right distal femur, talus, tarsal, and metatarsals; no intervention aside from physical therapy was done at this time. With the new diagnosis of AVN (avascular necrosis), the patient was referred to an orthopedic surgeon who’s only recommendation at this point is a total hip replacement of the left side with the possibility of the right side continuing to die and a replacement will be needed at the point the patient is no longer be bare weight or ambulate. She complains of constant discomfort and pain with extreme limited mobility. She is unable to adduct or abduct the left hip and cannot bend and raise left knee up. Patient physically has difficulty with activities of daily living including showering and getting dressed. Patient now makes use of a cane and is on a high dose of Morphine for pain control. Patient has been approved by orthopedic surgeon for surgery; however funding is not available at this time through her Indian Health Care.

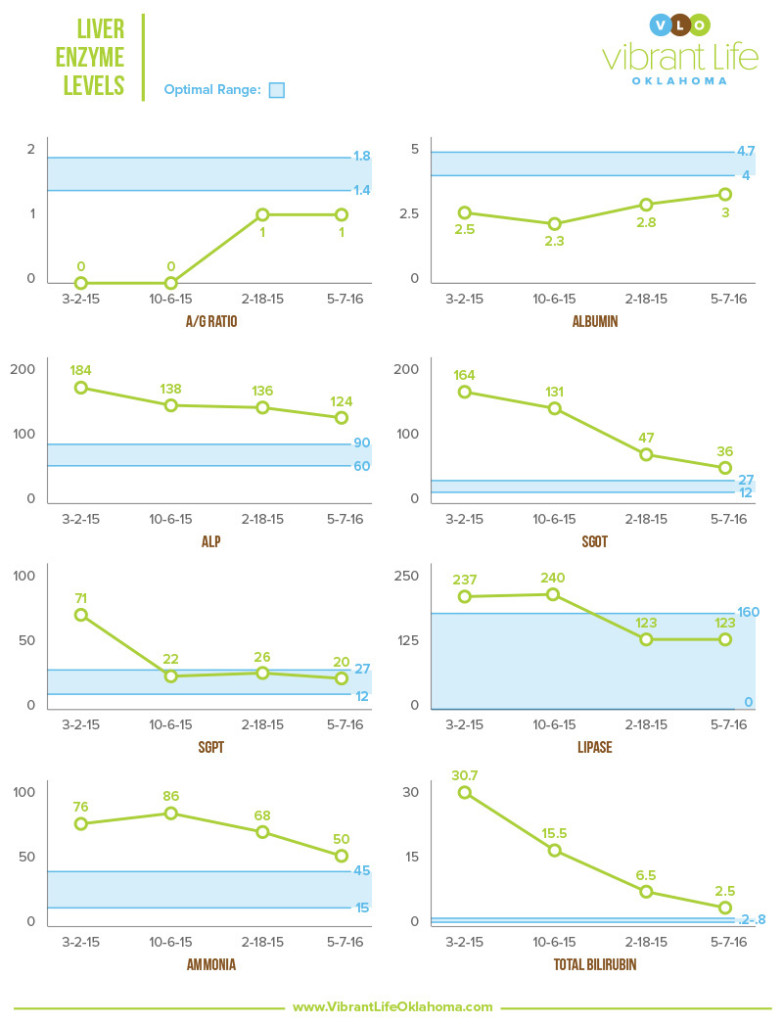
The following liver enzymes, ALP, SGOT, SGPT, and Lipase are enzymes that are released during organ damage, so the more organ (liver) damage, the higher the number.
A/G Ratio, and Albumin are blood proteins that are produced by the liver. Proteins transport hormones, vitamins, drugs and substances like calcium and magnesium. We want these numbers to increase, as that speaks directly to the function and health of the liver.
Ammonia is formed when protein is broken down in gut by bacteria. The liver converts ammonia to urea, so the lower the number the better.
Bilirubin is made in the body when old red blood cells are broken down. Bilirubin then travels to liver and is put into bile duct and stored in the gall bladder. High levels indicate poor liver function.
With the onset of the AVN and prescription of Morphine the patient’s liver is tolerating the medication well per lab results. R.M.’s skin has returned to a normal pink/pale color, the sclera of her eyes have only a minimal huge of yellow at the point of the mucous membranes. She now weighs 167 pounds, continues on vitamins; most importantly Vitamin C, Magnesium, L-Glutamine and Alpha Lipoic Acid. Regarding her diet she has added back in some dairy and dark berries. She continues to show improvement of bilirubin numbers and a stabilization of liver enzymes as seen in the following lab results.
AFTER TREATMENT:

On October 6th, 2015, I was contacted by Racheal’s mother at 6:00 am. She informed me that she had taken her daughter to the Emergency Room, that they were unable to start an IV on her to administer much needed fluids. So they sent her home. She Googled IV therapy and desperately called me, to see if there was anything I could do. To be completely honest I wasn’t sure if what I was being told was true, so I told her I would come and see her daughter, and assess the situation around noon that day.
After seeing Racheal for the first time it would not be possible to exaggerate how horrible her physical condition was. I found her blood pressure very low, and she was extremely dehydrated. swollen and retaining fluid around her ankles. She was also hallucinating, seeing things, and laid on couch for approximately two weeks. Every major organ group was compromised significantly, both her short-term and long term survival was very much in question. We started that her vascular system was in terrible shape, and starting an IV was a difficult task. Within a few days we opted to use her jugular vein which became our only option.
Raechel was on no medication, there was no other treatment being administered during this period of time from 10/06/15 until 07/2016. We administered the following substances two times daily, seven days a week. Alpha lipoic acid, glutathione, high-dose vitamin C, 60 grams or more. The patient’s diet was restricted to vegetables, fats, some protein, no sugar, no carbohydrates, nothing artificial. She was also given amino acid therapy to assist her with alcohol withdrawal
Essential oils were used, as well. Juniper was one essential oil that helped with the patient’s edema, and she applied that on the inner and outer sides of her palms. The juniper also helped elevate her mood. Frankincense was applied to the nape of the neck and to her head at night, to support immune function, and cellular receptor site balancing, to help with her addiction and mood. She also added lemon essential oil to her water, to support cleansing and detoxing.
There were two very distinct issues that the patient was dealing with; end stage liver failure, as well as alcohol dependence. They both had to treated at the same time. I’m happy to be able to say both issues are corrected today. She is living a normal life.
